Arthrosis
General information about joints
Although joints are differently constructed and have different ranges of motion, the basic principle of their construction remains the same.According to their weight burdening the cartilage thickness is different. In comparison to the ankle joint the cartilahge layers in the toe joints are relatively thin.
General information about joint cartilage
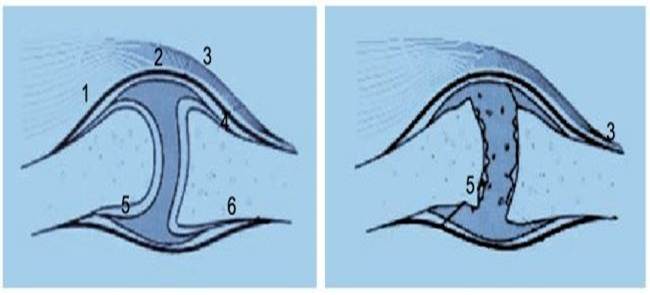
Joint bone Hyaline (elastic) join cartilage is thick up to 8 mm, this strength is found e.g. at the back of the patellar bone. Generally the stronger the burdening, the thicker the cartilage. In joint cartilage you don’t find vessels or nerves. The nutrition takes place by diffusion from the synovial fluid. In the joint a special cartilage (90 % hyaline cartilage with a strong water binding ability) is found. The cellular proportion in this cartilage is 1 – 10 %. The rest is the cartilage matrix, a special binding substance. Therefore the healing potential of the cartilage is severely restricted. There are only few cells, which have the ability to rebuild a new tissue. An existing defect will not be refilled or the refill will be done by replacement tissue (fibrous cartilage). This replacement tissue is not so durable like the original cartilage. Therefore an increased risk remains for an advanced joint damage and thus for arthrosis.
Arthrosis
This term includes degenerative changes of joints, which develop over the years. At the beginning there is always a joint damage, which leaves a cartilage with a diminished stress capacity. This is significantly rougher than healthy cartilage and leads to an increased cartilage wear in the joint, at first only by strong burdening, e.g. when doing contakt sports, later also by usual usual activities of daily life. The roughening or complete destruction of cartilage results in a stronger joint friction and the loss of its shockThe result is an increased burdening of the adjacent bone, because the cartilage absorption decreases. Hereby osteophytes (so-called bone attachments) in the joint are formed, which limit the joint additionally in its range of motion. Besides the upper ankle – mainly accidentially caused among others by fractures and repeated supination traumas – on the foot most of all the basic joint of the first toe (Hallux rigidus, Hallux valgus) but also the other toe joints (hammer or claw toe) are affected by arthrotic longterm consequences. Morning warm-up pain or run-in pain after a longer resting phase are relatively typical. Only in the further course pain occurs also after exercise or during nighttime. Living quality of the affected people will be gradually limited. The walking distance shortens, the sports load capacity decreases significantly and the participation in daily and work life is significantly restricted.
Rising life expectancy
With rising life expectancy the number of patients with higher and high age increases. This and the fact the joints are also strained more e.g. by a changed way respectively circumstances of life result in an increased consumption (degenerative change) of the affected joints, the final stadium being the arthrosis.
Therapeutic interventions
Today this frequent and fateful course can`t be inhibited by various therapeutical measures, but can be directed into acceptable ways. Especially here the PRP (Platelet Rich Plasma)-treatment with autologous growth factors as a new type of autologous blood therapy and the intraarticular injection of hyaluronic acid can be offered. By this on the one hand the painful shortening of the walking distance is functionally improved due to a better joint mechanism by better “lubrication”, on the other hand the time for more invasive measures like an arthroscopy (looking into the joint by endoscopic measures) or the implantation of an artificial joint can be delayed.
Course
What concerns the above listed injection therapies, 3 – 5 serial therapy sessions are needed. Important is the training of the adjacent and involved muscle groups consequently in order to achieve a better muscular joint guide. Thus the effects mentioned above are supported and preserved as long as possible. Additionally the Pulsating Magnetic field Therapy (PMT) can be performed to initiate the formation of new cartilaginous and bone tissue.