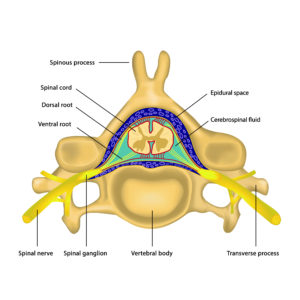
The term epidural infiltration describes the step-by-step injection of medication in the epidural space of the spinal cord, which is the space between the periosteum (bony skin) of the spinal channel and the spinal dura mater (hard skin of the spinal channel). This is illustrated in the anatomical diagram on the left using the example of the cervical spine.
All interventions are performed in the prone position. After manual palpation of the named anatomic landmarks local anesthesia is injected in the planned injection area under sterile conditions.
Now the infiltration cannula is inserted using resistance-loss-technique and by means of x-ray control which is fluoroscopy to the anatomic target region. The correct needle position will then be confirmed by injection of a contrast medium. After this the local anesthetics (e.g. Lidocaine, Bupivacaine) and water soluble glukocorticoide e.g. Kenacort are injected.
Epidural infiltrations are performed by us for several orthopedic disease patterns, among others for treating nerval root syndromes, lumboischialgia, coczygodynia, postdiscotomie syndrome and postfusion syndrome. In case of orthopedic operations also an epidural infiltration can be medically useful and helpful also for perioperative pain therapy. Besides the pain reduction first of all an earlymobilisation and functional therapy by the physiotherapist is made possible.
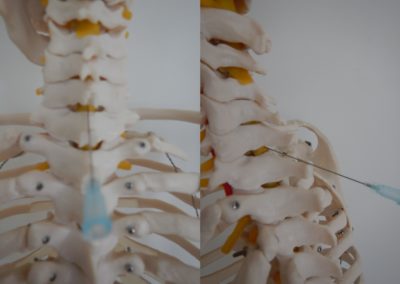
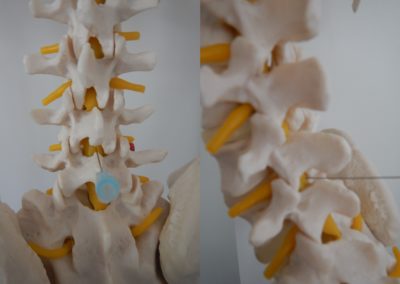
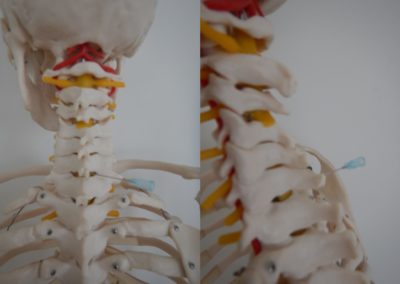
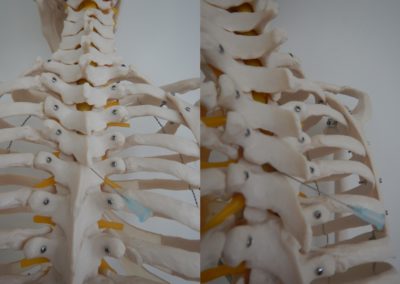
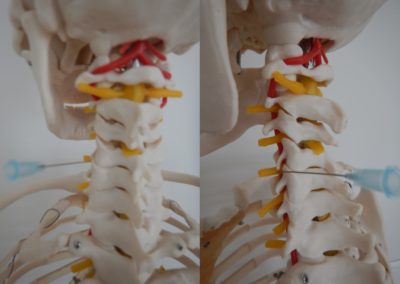
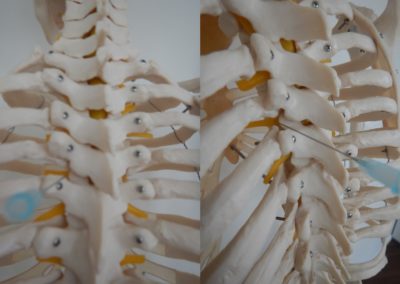
These preconditions result in different anatomic access routes and directions, which are demonstrated as follows on behalf of an anatomic model with 2 pictures each for comparison of cervical spine=HWS (on the left), thoracical spine=BWS (in the middle) and lumbar spine=LWS (on the right).
Interlaminar direct
Interlaminar oblique extraforaminal
Extralaminar direct transforaminal
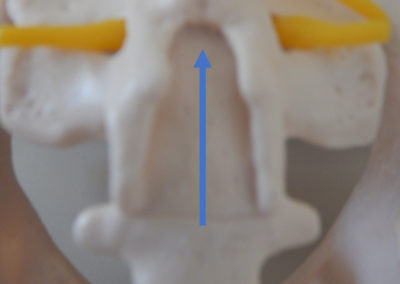
Hiatus sacralis (blue arrow)
Having the right indication these 3 techniques are a medically useful supplement for effective pain relief and for differentiation respective limitation and confirmation of the diagnosis stated before.
Typical complications
Infection
Vascular damage with bleeding and hematoma
Nerve damage with sensitive disorders, dysathesias and/or paresis
postspinal headache in case of accidential (unimposed) injury oft the dura or the spinal cord ending up in a so-called postspinal headache
Primary aggravation (worsening)with initial pain increase
Cardiocirculatory problemes with blood pressure decrease, increase in pulse rate, circulatory collapse and/or cardiac rest, pulmonary (lung) problemes with breathing disorders, pulmonary (lung) collapse (pneumothorax) and/or breathing rest
Insecurity of gait, coordinative disorders
Disorder of coordination and abilities to react (thereby no active participation in public traffic e.g. when conducting a car or riding a bicycle for 24 hours)
Due to the reasons listed above an accompaning person is mandatory for coming to and going home after the procedure and a follow-up appointment in our clinic on the following day for controlling of pain reduction and locomotor functions.
The definitive usually occurs within a few hours. In some cases, a new intervention is necessary, which can be repeated with a minimum interval of at least one week. The “Single-Shot-Therapy” method described here is as effective as the still commonly used catheter treatment in terms of efficacy and is even superior in terms of effort and logistics needed.